I have spent much of my career focusing on how data can be used to improve health. My journey to this topic came from pursuing improving patient care and population health through pioneering work in the development of primary care networks in Tower Hamlets and in the development of integrated care in North West London a decade ago. Through that experience, I saw the potential and the amazing power of linking data together to facilitate the design of new models of care, the enabling of it with the flow of information to support direct care, performance management and payment. These early efforts demonstrated material benefits for patients (including 15% reduction in the whole population non-elective admissions) and many things still talked about as somewhat radical (such as linking patient-level data across all forms of health and social care).
Looking more widely, I see the enormous potential and indeed progress that has been made not just in population health management and changing behaviour, but also in improving performance. But I am also acutely aware of the significant challenges that limit the progress wish to make. At an event with digital innovators (including Google Health, Babylon, MedoPad, Changing Health), NHS providers and NHSE participants clearly identified the main challenges as cultural, not technical.
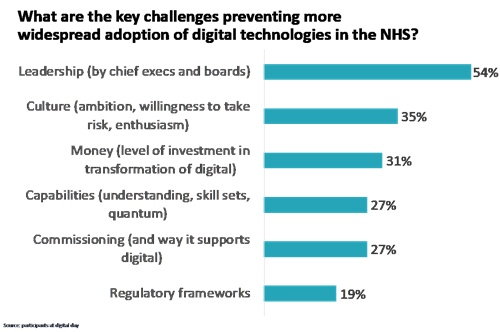
This reflects that there is insufficient leadership and attention to capturing the potential of analytics at the moment in the NHS. Too often issues, such as the tricky ones about information governance and data sharing, are put into the too difficult box. For instance, the fact that people today are still asking about the legal basis of sharing health and care data across primary care and social care illustrates this. The report of the Health Foundation also makes the point of the sizeable gap that exists in the application of healthcare analytics. It points out that the skills needed to deliver a robust analytical function include “statistics; manipulating and linking large data sets; social research methods such as survey design; mathematical skills (eg operational research and modelling); economics; epidemiology; methods and measurement; public health; improvement science; health policy; evaluation” and that these can’t all be found in teams of two or three people.
The CF way of thinking about healthcare analytics
At CF, when we think about data and analytics, we approach it as a way of creating the flow of information that supports change to happen. This enormous potential is created by the explosion of data and techniques to harness big data to apply machine learning and artificial intelligence. However, it faces many challenges to achieve this.
Value
Given limits in resource and capability, we need to focus on the things that are the most important and highest value. Too often the “use case” is unclear and there is insufficient consideration of where the value will be created. We always find it helpful with clients to start with clarifying the number one thing to focus on that will create value and pursue that first—as opposed to a list of 37 priorities. I recognise for the NHS as a whole or an industry as a whole it is impossible to focus on just one thing but it is really hard to make progress across multiple fronts at the same time.
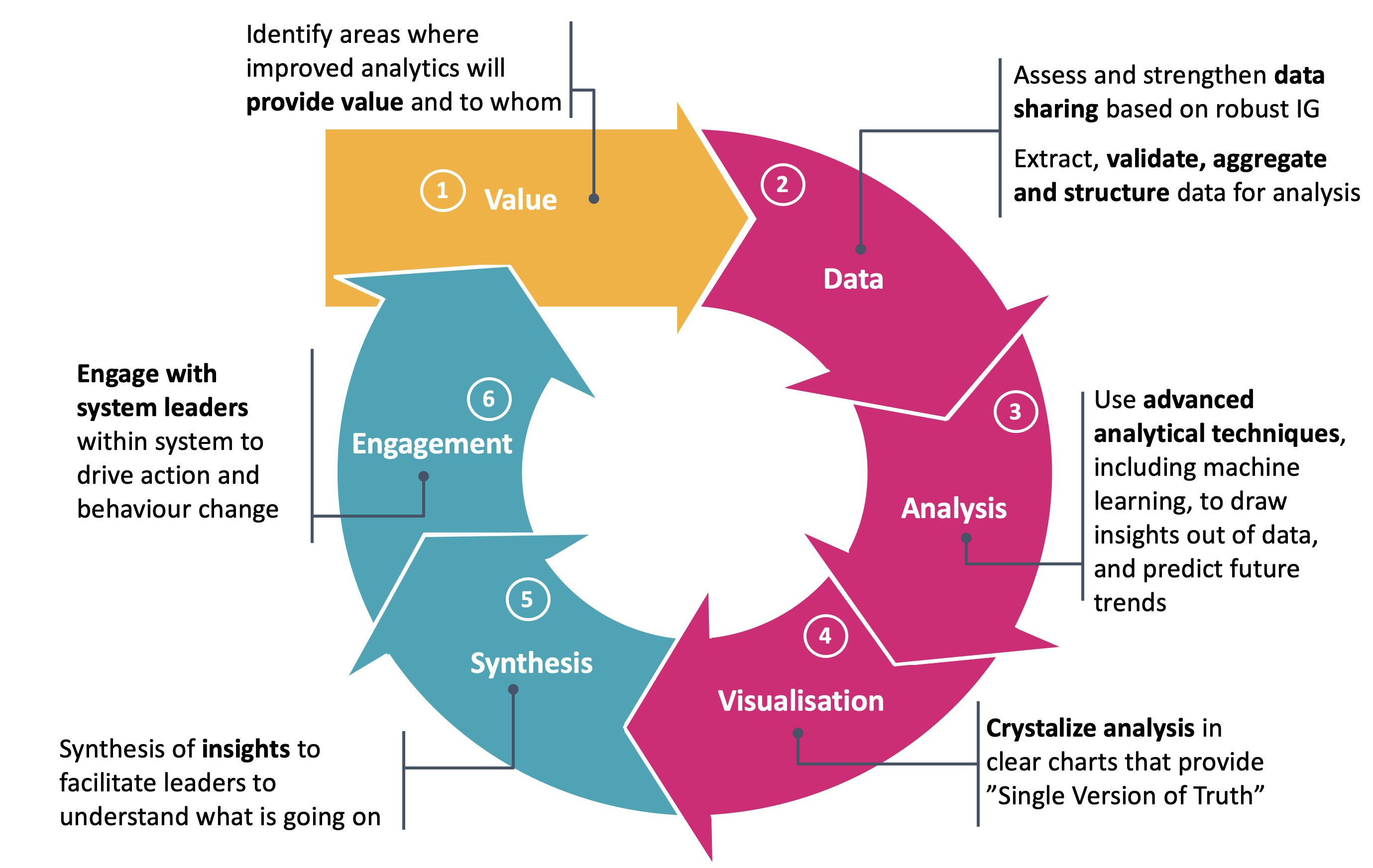
Data
Obvious to say it, the starting point of using data and analytics needs to be considering the data environment and how to unlock it. For me personally in my work as a consultant, this simple statement has been profound in meaning I start any work with asking about the data environment. This includes understanding three dimensions of data:
- depth
- scale
- longitude
It also means understanding the current agreements for data sharing, what is communicated about them to patients, and what the information governance arrangements are. It is crucial to get this right in order to have the trust of patients and those who control data on their behalf (either GPs or data protection officers in larger organisations). In doing so there is a need to be transparent about what the use of any data is and to engage. However, too often, the presumption is that data should not be shared or too high a bar is set (e.g., explicit consent) which entirely ignores the expectation that patients have that their data should be shared for their direct care, and that data can be anonymised and shared for legitimate purposes without explicit consent.
Analysis
Powerful analysis is now possible to identify risk, predict disease or activity, explore how to change, etc. Machine learning creates the possibility to see patterns that are too difficult to spot with the naked human eye – to stratify and target patients for interventions or to understand patterns of who might turn up when in the health care system. Artificial intelligence creates the possibility of acting independently (within parameters) to support interactions (e.g., with natural language queries with chat bots) through to support decision making (e.g., identifying likely cases of breast cancer) through to make and act decisions.
Visualisation
Doing great analysis is one thing, but to use it requires being able to visualise and communicate it clearly. Research by The Health Foundation shows the difficulty the NHS has in doing this. At CF, we focus on the creation of the “killer chart” that resonates with stakeholders. Unfortunately, a great deal of good analysis in the NHS never sees the light of day because it is unclear what it says.
Synthesis
Beyond simply a compelling chart, the critical question to ask is “so what?” What does the analysis mean? What are the implications for us? It sometimes feels like a chasm needs to be crossed from the world of analysis to its use and application for clinical or managerial practice.
Engagement
Engagement is a broad term often used within the health service to reflect the need to engage with clinicians, patients and wider stakeholders. Within the world of digital, there is another meaning in measuring who is engaged by the material, for how long and what do they do with it as a result. Both these meanings are critically important for data and analysis to have an impact. This is where the real value comes into play:
- Enabling a clinician to invite high-risk patients to an intervention
- Engaging a patient in the discussion of their condition
- Supporting clinicians and managers to look at the needs of their patients in a new way
- Supporting executives to manage a system in a different way
My question, having reviewed the amazing potential that data and analytics hold for healthcare, is when? When will this potential be realised? At the moment less than 10% of the country has access to linked datasets that allow integration of all health and care records together which is a starting point for understanding the needs of people holistically – when might there be universal coverage for them? At the moment who knows but perhaps 10 years. We need to not settle for that. People will be better able to look themselves and the health system better able to target, prevent, care for people with access to advanced analytics and this post-Covid period is a once in a lifetime opportunity to push forwards with an analytical revolution.


