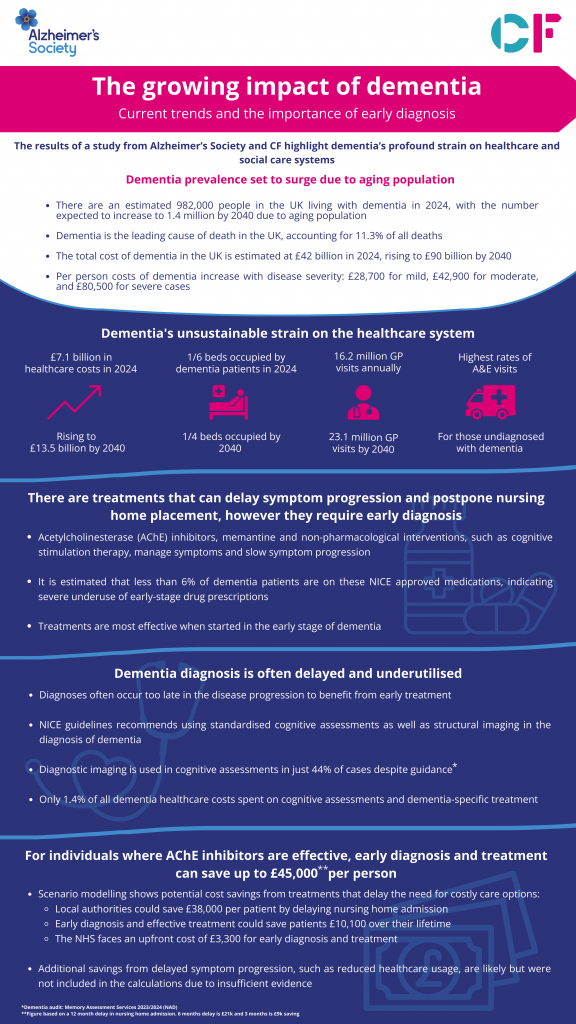
Dementia is now the leading cause of death in the UK, accounting for 11.3% of all fatalities. With an estimated 982,000 people currently living with the condition, this figure is projected to rise to 1.4 million by 2040. The economic impact is equally concerning, with costs expected to surge from £42 billion in 2024 to £90 billion by 2040.
CF was commissioned to investigate the social and economic impact of dementia in the UK. Using our advanced analytical tools, we leveraged a linked, record-level healthcare dataset from a Discover-NOW* database to develop a detailed understanding of the healthcare resource use of people with dementia.
Click to enlarge
Key Findings: The Burden on the Healthcare System
Our study highlights the significant strain that dementia places on the UK’s healthcare infrastructure:
- 36 million annual contacts across community, primary, and mental health services
- Nearly 1 million A&E visits by dementia patients
- On average 1 in 6 hospital beds occupied by dementia patients at any given time
These interactions lead to substantial costs. Healthcare expenditures related to dementia are currently £7.1 billion, which constitutes 14% of the total dementia-related costs. For 2024/25, with NHS spending estimated at £192 billion, dementia care costs make up 3.7% of the total expenditure, even though dementia affects just 1.42% of the population. The breakdown of healthcare costs is as follows:
- 47% allocated to secondary care, including hospital stays
- 21% to mental health services
- 13% to community care
- 10% to prescriptions
- 8% to primary care
Our analysis projects that healthcare utilisation by dementia patients will increase by up to 43% by 2040, pushing total healthcare costs to £13.5 billion.
Key Findings: Gaps in Diagnosis and Treatment
Despite the increasing burden, there remain significant gaps in diagnosis and treatment:
- Only 64.8% of people aged 65 and over with dementia in England receive a formal diagnosis
- Diagnostic imaging and neuro-psychology testing account for just 2% of all outpatient activities
- The current focus on diagnosing dementia in care homes—where the disease is often more advanced—limits opportunities for early intervention
- Less than 6% of dementia patients are on these NICE approved medications, indicating severe underuse of early-stage drug prescriptions
The Case for Investment in Early Interventions
Investing in early and accurate dementia diagnosis is critical for multiple reasons. It enables timely interventions that slow symptom progression, reduce the need for intensive care, and significantly enhance patient quality of life. Additionally, early interventions can help reduce the long-term strain on healthcare resources.
Our study uses scenario modelling to assess potential cost savings from early diagnosis and treatment. The results show that early intervention could delay care home placements by an average of 12 months, generating savings of £8,800 to £44,900 per person by postponing the need for expensive nursing home admissions.
Please contact us today to find out more about this research and our work in data, digital and RWE.
*Discover-NOW database. (Accessed 2024). https://discover-now.co.uk