Dementia is one of the UK’s most pressing health and social care challenges, with profound impacts on individuals, families, healthcare systems, and the economy. With nearly one million people in the UK living with dementia, more needs to be done to ensure its impact on those affected, the healthcare system and the economy is realised and prioritised.
In support of World Alzheimer’s month, CF has summarised its recent work with Alzheimer’s Society to understand dementia’s growing impact and the critical importance of early diagnosis and intervention. CF applied a unique data-led, real-world evidence approach to deliver three reports on the impact of dementia:
- Annual cost of dementia (see summary report here)
- Dementia’s contribution to health metrics (see report here)
- Impact of early diagnosis and treatment (see report here)
The headline figures are sobering and present significant structural and financial challenges to the UK.
Growing prevalence and annual costs
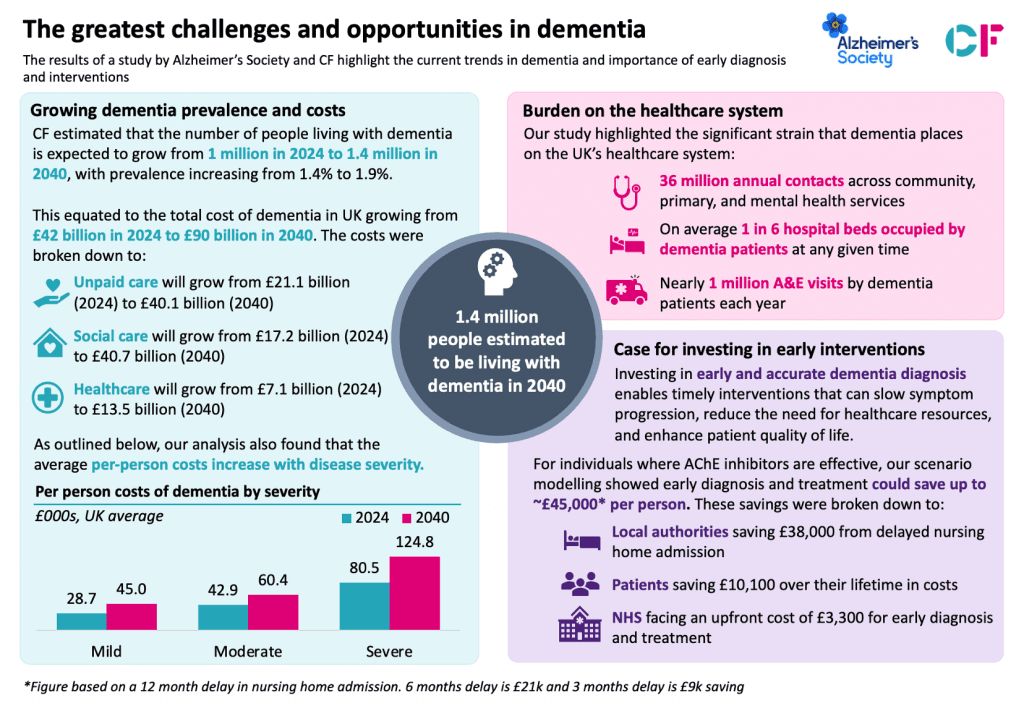
Using our advanced analytical tools, CF leveraged a linked, record-level healthcare dataset from a Discover-NOW* database to develop a detailed understanding of the healthcare resource use of people with dementia. Our study found that the number of people living with dementia in the UK is projected to rise from nearly 1 million in 2024 to 1.4 million by 2040. With the number of people with dementia expected to grow, it is not surprising that the forecasted cost of dementia is expected to rise from £42 billion to £90 billion over the next 16 years. The key costs were broken down to:
- Unpaid care growing from £21.1 billion (2024) to £40.1 billion (2040)
- Social care growing from £17.2 billion (2024) to £40.7 billion (2040)
- Healthcare growing from £7.1 billion (2024) to £13.5 billion (2040)
Unfortunately, 63% of these costs are borne by patients and their families, with 41% reporting financial difficulties. We found that the average per-person costs vary greatly with disease severity, with mild dementia costing £28,700 per year whilst severe dementia can cost up to £80,500. These costs likely only represent a small proportion of the total cost of care as unpaid care constitutes to 50% of total costs in 2024. Unpaid carers play a critical role in supporting people with dementia, with one third reporting to spend over 100 hours per week on caregiving duties.
Burden on the healthcare system
CF identified that dementia is also placing substantial strain on the UK’s healthcare system:
- 36 million annual contacts across community, primary, and mental health services
- Nearly 1 million A&E visits by dementia patients
- On average 1 in 6 hospital beds occupied by dementia patients at any given time
The strain that dementia places on the UK’s healthcare infrastructure further increases with disease severity. People with severe dementia had an average length of stay in hospital for unplanned admissions that was more than three times longer than people with mild dementia. Total bed day utilisation amongst people with severe dementia was also found to be more than twice as high as people with mild and moderate dementia.
By 2040, it is estimated that the UK will require an additional 100,000 care beds to adequately meet the needs of people with dementia. This must be coupled with more specialised care that is tailored to the varying stages of dementia. However, over the last 5 years the supply of care beds has decreased, with construction costs also not being compatible with current achievable fee rates (outside of the self-pay market). Targeted investments in areas with higher concentrations of dementia cases will therefore be essential to ensure equitable access to care across the UK.
With the increasing prevalence of dementia likely to be clinically and financially unsustainable for the UK, innovations in care and treatments for dementia are also required. There is hope for the future, with Disease Modifying Treatments for Alzheimer’s disease on the horizon. It has been well established that whilst there are several benefits of DMTS and non-pharmacological interventions (NPIs) such as diet, exercise, and cognitive stimulation, the benefit of these interventions are dependent on early diagnosis.
Case for investment in early diagnosis and interventions
With only 65% of cases in the UK currently being diagnosed, there is a need to increase the early diagnosis capacity. Currently only 2% of all outpatient activity is diagnostic imaging and neuro-psychology testing. Research has found that undiagnosed patients with dementia attended A&E 1.5 times per year. This is more than people with a diagnosis for mild, moderate and severe dementia and 3x more than people without dementia. Without investing in increasing diagnostic capacity, undiagnosed people with dementia will continue to have high healthcare utilisation.
Investing in early and accurate diagnosis enables timely interventions that slow symptom progression, reduce the need for intensive care, and significantly enhance patient quality of life. Early interventions have been shown to reduce the long-term strain on healthcare resources, with savings of £44,900 per person when nursing home admissions were delayed by an average of 12 months through effective management and treatment of Alzheimer’s Disease.
The cost savings from earlier diagnosis and treatment will likely to be shared across both people with dementia and the public. It is therefore essential that the NHS and broader government prioritises dementia in policy and decision making, thus allowing people with dementia to access to novel therapeutics and ensure key infrastructure, such as diagnostic and imaging equipment, is in place to allow for treatments to take place.
Our findings suggest a pressing need to influence policy and drive change across the following five areas:
- Improving early and accurate dementia diagnosis to empower individuals in managing their health, making informed future plans, and accessing timely treatments that improve quality of life.
- Adopting existing and innovative therapies to delay dementia symptom progression, providing both improved patient outcomes and cost-saving opportunities across the UK healthcare system.
- Increasing investment in and support for unpaid carers, recognising their critical role in dementia care and ensuring they have the resources, respite, and training necessary to sustain their commitment.
- Advancing social care reform to enable the delivery of high-quality and person-centred care for people with dementia.
- Enhancing data collection on dementia progression and care, enabling more effective monitoring, research, and improvement of care practices, while supporting better policy-making and resource allocation.
Please contact us today to find out more about this research and our work in data, digital and RWE.







