Integrated Care Systems (ICSs) were formed to coordinate provision of services to improve health outcomes, tackle inequalities in outcomes, experience and access, enhance productivity, and support broader social and economic development. In July 2022, the Integrated Care Boards (ICBs) were formalised as statutory bodies and 42 ICBs were established across England. By December, Integrated Care Partnerships (ICPs) within ICSs are expected to publish an integrated care strategy detailing the needs of their community, and where system partners can work together to meet those needs (see our summary here). The integrated care strategy is an opportunity for ICPs to set out evidence-based priorities aimed at improving public health and wellbeing and reducing health inequalities. This is occurring in the context of greater pressure on finances in the public sector and against a wider backdrop of a cost-of-living crisis that most strongly affects those already struggling.
There is a wide body of evidence that underlines the relationship between deprivation and health outcomes, but this has always been challenging for any one agency in a care system to act on alone. Systems involving the NHS, local authorities and Voluntary, Community and Social Enterprise (VCSE) organisations now have an opportunity to work together to change this. Together they can address the wider determinants of health outcomes, starting with the impact of deprivation.
Our analysis has found that:
- There are many health-related metrics, such as number of preventable deaths, that increase as deprivation increases
- There are also several health-related metrics including life expectancy and those receiving support from GPs, which decrease as deprivation increases
- Many health-related metrics for instance people taking up NHS Health Check invitations and access to NHS dental services do not correlate with the level of deprivation
Getting a better understanding of these relationships can help to underpin strategies to improve them and drive improvements in population health.
Firstly, some measures are highly positively correlated with the Index of Multiple Deprivation (IMD). This means that as the level of deprivation increases, the measure also increases (see Figure 1 below). These measures can be things we generally see too much of in areas with high deprivation.
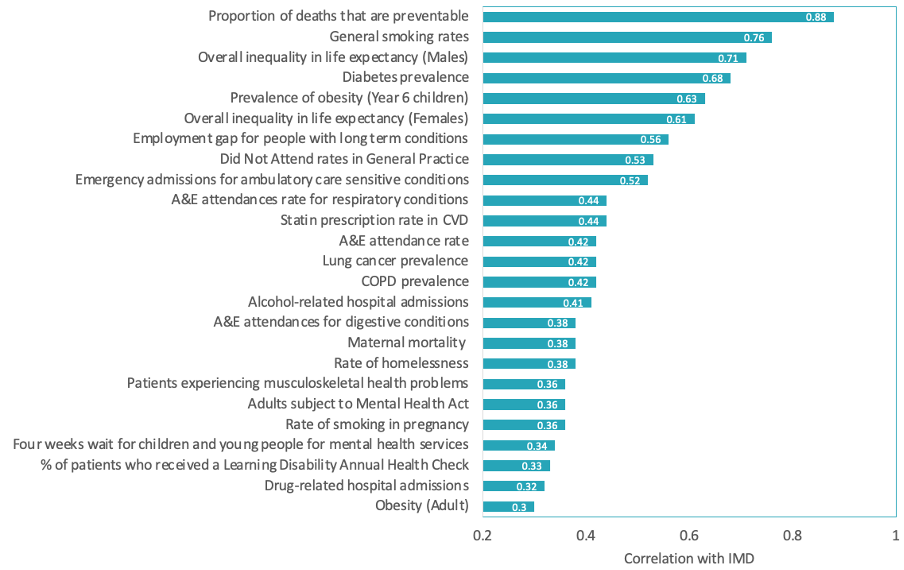
Figure 1: Metrics positively correlated with IMD.
For example, ‘deaths from causes considered preventable’ is the measure most highly correlated with IMD, with a correlation coefficient of 0.88. Preventable deaths are defined as deaths that can be mainly avoided through a combination of healthy behaviours, effective public health, and primary prevention interventions. To address this inequality, we must ensure areas of high deprivation have sufficient preventative services such as public health measures and primary care in place. Equally, smoking, diabetes, obesity in children, the use of secondary care services such as A&E and the use of inpatient mental health services are all strongly associated with deprivation.
Secondly, some measures are negatively correlated with IMD, meaning that as the level of deprivation increases, the measure decreases (shown in Figure 2). These measures highlight that some of the most important preventative and proactive interventions are not sufficiently taken up or not offered to meet specific population needs in areas of high deprivation.
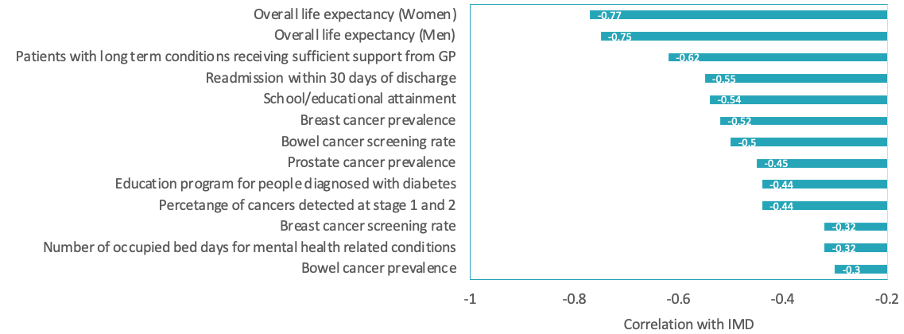
Figure 2: Metrics negatively correlated with IMD.
For example, a lower proportion of patients living in deprived areas have their cancer detected at stage one and two. This may be explained by people in areas with more deprivation having:
- Greater difficulty in securing time off work
- Less convenient access to care with reliance on public transit
- A longer waiting time for treatment, with analysis into consultant-led referral to treatment waiting times finding that waiting lists in the most deprived areas have increased by more than half since the pandemic
- Less confidence in articulating the importance of having appointments in face of any delays
- Potential language barriers faced in rescheduling appointments
- Lower awareness of the significance of acting on signs of cancer quickly
We also see a negative correlation between deprivation and the use of services such as Diabetes Education programs, screening programs for breast and bowel cancer, and patients receiving sufficient support from local services to manage their long-term conditions. With higher levels of deprivation, lower use of these services and lower rates of patient’s receiving sufficient support are seen.
We also see a wide range of measures that have simply no relationship with deprivation. We have identified a set of measures across the pathway looking at access and outcome measures aligned to the three areas of the integration across ICSs: community based and hospital based care, health and social care and physical health and mental health. We illustrate these measures in Figure 3 below:
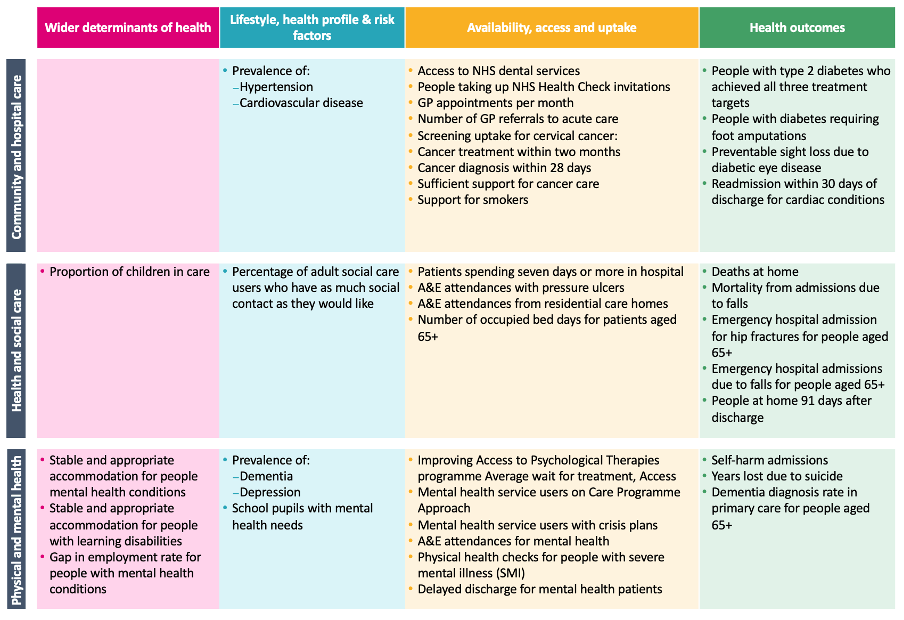
Figure 3: Metrics not strongly correlated with IMD
We mention this as there appears to be no obvious link with deprivation and hence every reason to think that these can and should be addressed in any area.
Improving outcomes in areas with high deprivation
Some important conclusions from this analysis are:
- Prevalence of many long-term conditions is strongly associated with deprivation, including diabetes, obesity, COPD, and lung cancer
- Preventative measures including cancer screening and diabetes education are negatively associated with deprivation (meaning they happen less than they should do)
- Some outcomes are not strongly associated with deprivation
- It’s even more important to understand what this looks like at place and neighbourhood level – overcoming the inequalities shown by this analysis will require engaging and working closely with people in local areas to determine how best to address inequalities locally
There is the potential to change these outcomes, and we believe the following seven actions are important in reducing health inequalities:
- Improving data quality and recording: changing how data is gathered both nationally and locallyould improve transparency
- Understanding local need and targeting best support: asking residents and providers what services are needed
- Contact points/ leverage points: making use of points of contact in the community
- Culturally appropriate communications: reaching the wider community using the best methods and correct messaging for awareness
- Access point issues: removing obstacles around capacity and ease of booking appointments and embracing virtual alternatives for those unable to travel
- Engaging of local providers to address propensity to refer
- Workforce reflecting local community: are there enough staff in the services to deliver care
While these actions provide the opportunity to reduce some health inequalities, it is important to understand that each ICS is starting from a different position. The policy changes appear to have recognised this – with all ICSs having to develop an integrated care strategy that sets out measurable objectives that should be targeted across the system, and a timeline against which they should be delivered. The challenge for local systems will be to select the objectives that will impact on population health the most – and to develop a realistic plan to achieve these objectives.
Our Insights and Collaboration Engine (ICE) platform supports end-to-end planning – setting objectives and measuring improvement and impact. Contact [email protected] now to get a free demo of the tool.


