Dementia is one of the biggest healthcare challenges of the 21st century, affecting millions worldwide. In the UK, nearly 1 million people are currently living with dementia, a figure projected to rise to 1.4 million by 2040. In the United States, more than 6 million people suffer from dementia, and the condition is responsible for over 100,000 deaths annually. Dementia also carries a substantial economic burden, with total costs exceeding $600 billion annually in the United States. As populations age, healthcare systems worldwide are bracing for what was once feared to be an impending “tsunami” of dementia cases.
However, new research suggests a more nuanced reality. While the total number of dementia cases is increasing due to population ageing, the incidence rate—the likelihood of developing dementia at a given age—has been steadily declining for decades.
Declining dementia incidence
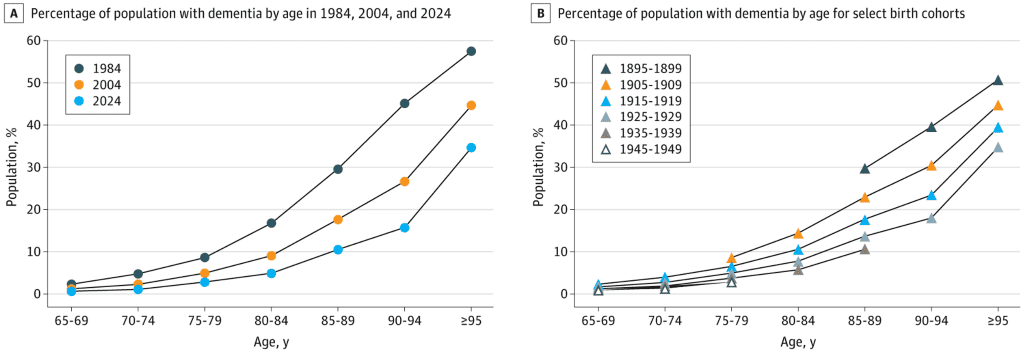
A comprehensive analysis of three large population-based studies found that the age-adjusted prevalence of dementia has decreased by two-thirds over the past 40 years (Stallard et al., 2025). The data revealed a staggering 67% drop in dementia risk at any given age over this period. For instance, in 1984, 30% of people aged 85–89 had dementia; by 2024, this figure had fallen to just 10%. Additional analysis of the data also revealed that each successive five-year birth cohort has a lower risk of dementia at a given age than did their predecessor.
Figure 1: Percentage of the US population with dementia by age in 1984 vs 2004 based on National Long Term Care Survey data.
If current trends continue, dementia prevalence is expected to rise by 25% by 2050, driven by a doubling of the older population. Supporting this projection, a previous analysis from researchers in the Netherlands, using data from the Rotterdam Study (Brück et al., 2022), estimated that dementia cases in 2050 would be 30% higher than in 2020. These findings highlight the complex interplay between declining individual risk and an ageing population, reinforcing the need for robust healthcare planning and investment in dementia care and prevention.
Similar trends have been observed globally, particularly in high-income countries. Researchers have attributed this decline to several key factors:
- Better cardiovascular health – Improved management of hypertension, diabetes, and cholesterol, along with reductions in smoking rates, have significantly reduced dementia risk.
- Higher education levels – Increased access to education has been linked to greater cognitive reserve, helping individuals better withstand brain changes associated with ageing.
- Healthier lifestyles – Improved diets, increased physical activity, and greater awareness of brain health have all contributed to lowering dementia incidence.
These findings challenge long-standing assumptions about an inevitable explosion in dementia cases. However, they do not mean that dementia is becoming less of a public health issue—quite the opposite.
Rising dementia prevalence
Despite the encouraging decline in dementia incidence, the total number of people living with dementia continues to grow due to population ageing. According to the National Institute on Aging (NIA), the number of new dementia cases in the U.S. is projected to nearly double, increasing from approximately 514,000 per year in 2020 to around 1 million per year in 2060. This reflects the demographic shift as larger cohorts reach old age, where dementia risk is highest.
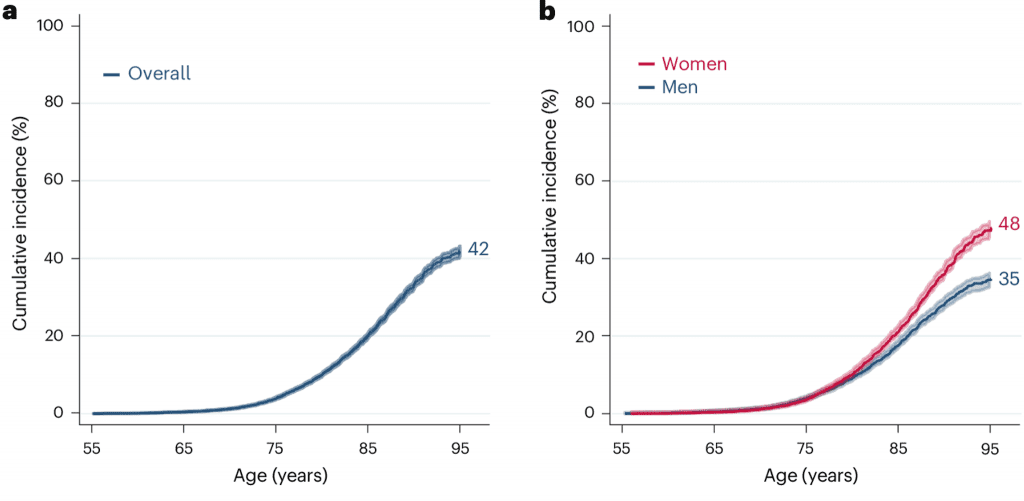
A crucial aspect of this trend is the sharp increase in lifetime dementia risk estimates. Previous studies suggest that 11–14% of men and 19–23% of women in the United States will develop dementia during their lives. A recent study now estimates that after the age of 55, an individual’s lifetime risk of developing dementia could be as high as 42% (Figure 2), more than double previous estimates (Fang et al., 2025). Specifically, the risk of dementia was 4% by age 75 and 20% by age 85, with the majority of the risk occurring after 85. Certain groups were found to be more at risk than others. For example, women had a higher lifetime risk due to survival to older ages, 48% versus 35% in men (Figure 2). People with two copies of the APOEε4 allele had a lifetime risk of almost 60%, versus 48% for those with one copy and 39% for those with none.
Figure 2: Lifetime risk of dementia (a) overall and (b) in women and men.
This suggests that even with a lower per-person risk at any given age, the sheer number of older adults means dementia will continue to strain healthcare systems. This highlights an urgent need for policies that promote healthy aging. Additional interventions targeted towards high-risk individuals may also help reduce the societal cost of dementia.
What does this mean for healthcare strategy?
This dual trend—lower individual risk but a higher overall burden—has profound implications for healthcare planning, research, and policy. Key considerations include:
- Equity in prevention – While dementia risk has declined in wealthier and more educated populations, disparities remain. Policymakers must ensure preventative interventions, such as cardiovascular care, education and lifestyle interventions, are available to all people who are at risk of developing dementia.
- Healthcare capacity planning – Memory clinics, specialist dementia services, and community-based support will need to expand to accommodate increasing demand, even as prevention efforts continue.
- Policy and funding shifts – Dementia is becoming one of the largest drivers of healthcare costs. Policymakers must now balance investment in prevention with expanded dementia care services and support for care gives.
These findings highlight the importance of data-driven, forward-thinking planning in dementia care. While the future of dementia is not set in stone, it is clear that proactive measures are needed to support both prevention and care for those affected.
To learn more about our work in dementia care and healthcare strategy, contact us.