Executive summary
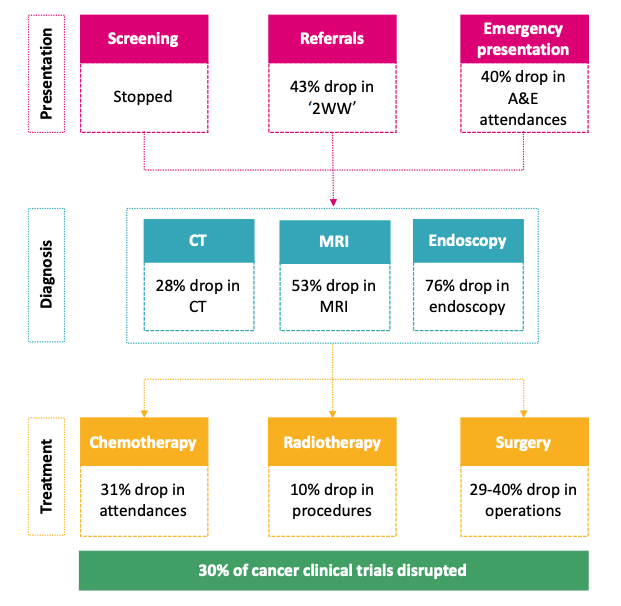
It is becoming increasingly clear that one of the biggest threats to health in the UK brought on by the COVID-19 pandemic, apart from COVID-19 itself, is to cancer services and cancer patients. The major disruptions to the cancer pathway have effectively stopped cancer screening, reduced referrals by more than 40%, and as a consequence have impacted considerably on cancer diagnosis and treatment, (including surgery, chemotherapy, and radiotherapy). In addition, there has been a major disruption to clinical research activity, including access of patients to innovative clinical trials.
These gaps and the overall challenge have been recognised by NHS England and the response has been to put cancer as the top priority for NHS planning for the rest of this year, in the guidance issued on July 31st. This announcement clearly demonstrates that the NHS and the government are seeking to address the challenge. However, the scale of the challenge is large and widespread and, hence, we have sought to help paint a detailed picture of the current position and what should be done to respond in the best interest of citizens and patients.
Inevitably, the slowdown in activity that has been experienced will lead to delays in the detection and treatment of cancer, which in turn can be expected to adversely affect cancer outcomes. As a result of these delays, the NHS’ stated desire to increase early stage detection from 44% to 75% could be set back to 42%, potentially reversing years of progress.
The worse outcomes associated with later-stage detection may lead to nearly 3,600 for 3 months of disruption and 7,200 excess deaths for 6 months of disruption this year for the cohort of patients whose cancer care is disrupted. Taking the reduction in urgent referrals of citizens to cancer diagnostic services as a starting point, we modelled the anticipated change in the distribution of diagnosis by stage. Patients who are detected at later stages will have lower chances of survival, which implies that overall survival rates will drop. This analysis is consistent with other findings recently published, suggesting a range of 1,412 deaths for one month of assumed disruption to 9,280 deaths for six months of disruption.[i]
The impact of the COVID-19 disruption of cancer services could also be expected to lead to changes in five-year survival—potentially setting the UK’s progress back by up to 8 years, and render its survival rates comparable to poorer performing countries such as New Zealand, Turkey, and Lithuania for the period 2010-2014 (ignoring any impact of COVID-19 on survival in those countries).
In light of these findings, it has become evident that restarting cancer as rapidly as possible is urgent, as well as ensuring minimal disruption to activities in the event of further COVID-19 peaks. Perhaps the most critical step is to restore confidence and make patients feel safe in presenting to their GP or specialist services if they show any potential signs of cancer. The “Phase III Letter” from NHS England lays out mandatory steps to address cancer, listing it as the first priority for recovery. Broadly, the actions are all in the right direction including an imperative to recover to 100% of usual volumes in Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and Endoscopy. We would note that recovery to this level will be demanding, but in reality will need to go further and exceed pre COVID-19 levels so as to reverse the consequences highlighted above.
We have outlined the necessary steps to recover and restore cancer services, namely creating safe diagnostic hubs for patients, increasing diagnostic capacity (CT, MRI, and endoscopy), dramatically increasing rapid testing for patients and staff, and working with GPs to better understand and address the bottlenecks. Creating COVID-secure diagnostic hubs will require:
- A 131% increase in diagnostic capacity (CT, MRI and endoscopy) over the period of 3 months
- 124,000 to 172,000 additional COVID-19 tests per week for patients and staff to give confidence that cancer services are COVID-secure
- 305,000 urgent referrals per month for a 6-month period, with the attendant encouragement of patients to present to GPs and GPs to refer to specialist cancer services
There are a number of challenges to be resolved in order to achieve the ambitious goals that we have set, including: 1) the scale and urgency of capacity response, 2) the shortage of available capacity in the NHS, 3) the delays and gaps in data, and 4) ensuring sufficient funding.
Similar challenges were overcome in the NHS’ response to COVID-19 – and a similar breadth and scale of response will be needed to address cancer. This will require a massive surge in activity and capacity, which needs to be implemented in each Integrated Care System (ICS), in each cancer alliance, and between providers in the NHS and the independent sector. We suggest that this entails: 1) developing a detailed demand and capacity view for each ICS and alliance (across the NHS and independent sector), 2) setting-out a detailed workforce plan, 3) expanding data flow, and 4) securing sufficient funding to enhance our future health.
To read the full article, click here
[i] Sud, Torr, Jones, Broggio, Scott, Loveday, Garrett, Gronthoud, Nicol, Jhanji, Boyce, Williams, Riboli, Muller, Kipps, Larkin, Navani, Swanton, Lyratzopoulos, McFerran, Lawler, Houlston and Turnbull, Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study, The Lancer Oncology (July 2020): https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(20)30392-2/fulltext


