Leveraging increased returns on our collective investment
The Value in Health series from the NHS Confederation and CF explores the potential of the health and care system through understanding, researching and modelling the positive relationship between increasing NHS spending, health outcomes, and economic activity. The first report set out that every pound invested in the NHS yields approximately £4 back to the economy. The subsequent reports found that spending this in primary and community care yielded even better returns at £14 per £1 spent for those places who are spending less relative to needs. This report pushes further into understanding return on investment (ROI) at intervention level and the implications for the health and care sector—and responds to questions many had about what specific interventions have the highest ROI?
Focusing on higher impact interventions
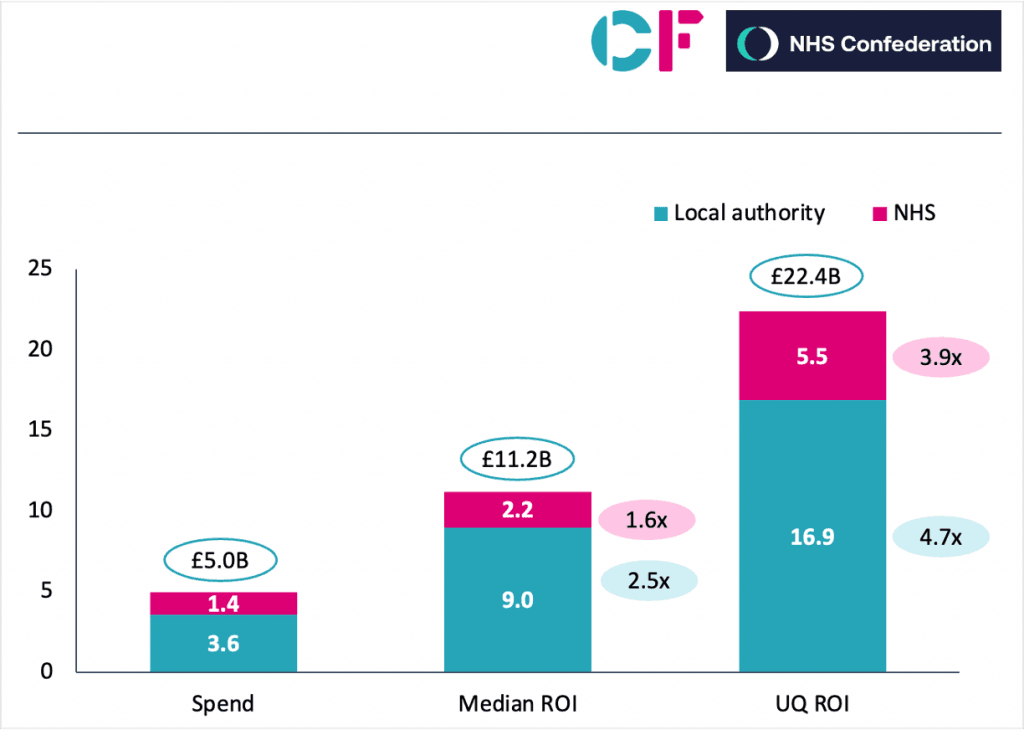
Prevention could have much bigger impact interventions were selected with the highest returns. A conservative estimate suggests £11bn more savings per year could be achieved from the £5bn currently spent on the public health grant by local authorities and on health inequalities by the NHS via Integrated Care Boards. Analysis of the ROI across the interventions in this report highlight a typical median return for an NHS intervention of 1.6 and for a local government intervention of 2.5. Focusing on higher impact interventions and if the scope of spending that used ROI in decision making was increased or more investment was made in prevention, this opportunity would scale and could be bigger.
Impact from investment in prevention, £billion
NHS and Local authority opportunity targeting median and upper quartile return on investment
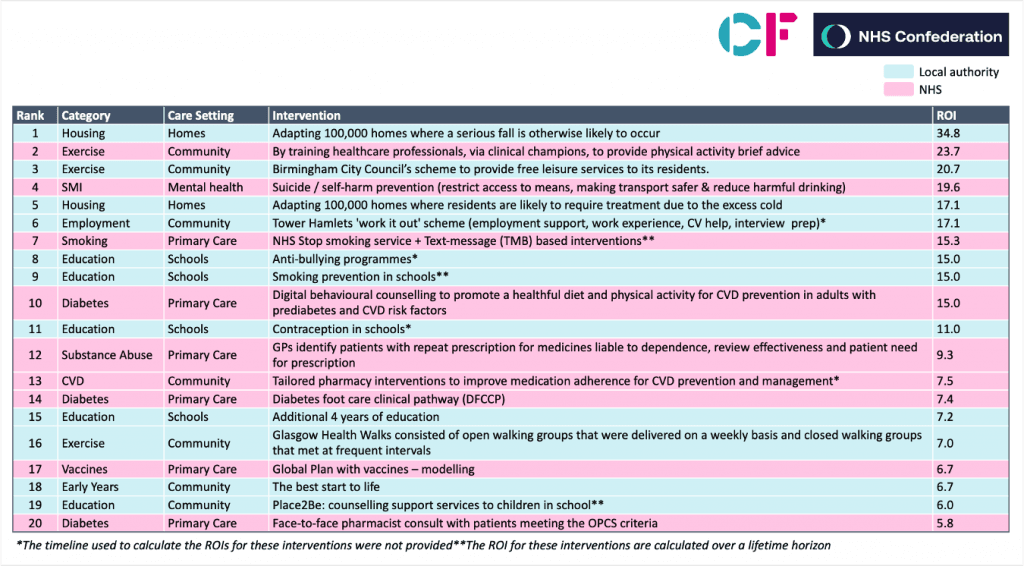
The evidence is clear: the top 20 interventions by ROI were all community-based with a range of returns on investment from £6.90 to £34.75. This further reinforces the key messages from the previous Value in Health research and highlights the importance of consistent working across NHS, local government and other partners.
Top 20 interventions by category and care setting
Taking a systematic approach
The other critical finding is that there should be efforts more systematically evaluate and apply an approach that incorporates both population need and getting the very best value for money. There is significant variance in ROI between interventions, both within intervention categories and between studies of the same intervention type. The intervention that is chosen is therefore of material importance and an evidence-based approach is essential. For both NHS and local authority colleagues responsible for commissioning services, the consideration of ROI in decision making should be as important as the needs of the population. By way of example, for secondary prevention of cardiovascular disease, the ROI ranges from £0.34 to £7.52 – with the highest gains from community pharmacy based detection.
One particular area of note was the impact of intervention on children and young people – including those related to education. Of the top 20 interventions, six were related to education or early years. When considering ROI by age, we found there was no variance by age for interventions, with many studies not considering the impact of the intervention beyond more than five years. The implication of this is that investment in children and young people returns at least as much as older people and is likely to exceed the stated ROI given the lasting effects of childhood health on adult health, employment and socioeconomic status.
The underpinning research amounts to an impressive evidence base that will be of wide interest for health and local government leaders. Discussions with ICB’s and local authorities suggest that informed decision-making is not happening in the way it should. In response, the NHS Confederation and CF have developed a six-case framework (pg 26) for those working in health and care to consider the economics of health in investment decisions. We strongly recommend this framework is embedded in everyday decision-making on prevention.
This report’s recommendations centre on four thematic areas for national government, NHS England, integrated care systems and local authorities:
- Invest more in prevention, particularly where we know it has impact, for example children and young people,
- Take an evidence-based approach to commissioning services that considers ROI as part of holistic assessment,
- Use data to systematically evaluate and benchmark interventions, leveraging the longitudinal data available to the NHS and the investment in Secure Data Environments and the Federated Data Platform.
If the current approach taken to investment is not changed, we believe the current pathway will lead away from the evaluative learning health system approach that is a critical part in delivering prosperous, preventative places and improving population health outcomes.
Context to the report
The recently published ‘Independent investigation of the NHS in England’ by Lord Ara Darzi has stated that despite a consistent intent to spend more money on prevention and in the community as opposed to in the acute sector, the opposite of this has been achieved. The Prime Minister and Secretary of State for Health and Social Care have also now said the NHS must reform or die. Three big shifts are anticipated as part of the 10 year NHS Plan: from analogue to digital, from sickness to prevention, and from acute to community.
However, as Darzi points out the inverse of this intent has been achieved. Spend on acute care has risen from 47% in 2002 to 58% in 2022 while primary care has fallen 27% to 18%. Hence, investing more in prevention will require reversing this trend—and needs to recognise it is not simply intent that matters but it is critical that this follow through in practice in each ICB and is underpinned by enablers of data, commissioning and management capability that is aligned behind this intent.[1]
It is no coincidence then, that this final report in the series is published at another time of significant national turmoil and when the issues in this report are firmly on the minds of NHS and local authority leaders. This work explicitly addresses two of the three reforms needed, and makes a clear case for shifting to a more proactive and preventative healthcare system through community based interventions.
Historically, there has been a significant amount of research and policy published related to prevention and the social determinants of health. While there is an acceptance that it is critical for the sustainability of the health and care sector, and some green shoots of localised practice are certainly showing, this wealth of evidence that has been built up over time has clearly not yet translated into material shifts in what we spend money on and how systems work. Service spend and delivery across the health and care sector over the last ten years demonstrate this point and there are many reasons for this. A lack of discretionary spend; repeated cuts to local authority budgets, including the funds reserved for public health; the pandemic and the subsequent operational pressures have all directed attention and resources away from proactive care, yet for many this issue remains the north star.
In the previous reports, innovative research and modelling has highlighted the strong economic and system basis for investment outside of the hospital. This report sets out a compelling story, but more remains to be done. In this report, the existing evidence base for preventative decision-making has been re-examined, linking both NHS and local authority budgets, which interventions we should value the most understood, and a framework that can tangibly help integrated care boards (ICBs), providers, local authorities and policy makers to consider what should be done for their local populations has been set out. We believe that embedding this framework into ways of working, coupled with national bodies taking forward some of the recommendations we set, will help pave a new pathway towards prevention.
We hope this report, and indeed the broader series, is both practical and useful to the full range of interested parties.
[1] https://www.gov.uk/government/publications/independent-investigation-of-the-nhs-in-england
About NHS Confederation
The NHS Confederation is the membership body that brings together and speaks on behalf of organisations that plan, commission and provide NHS services in England, Northern Ireland and Wales. The members we represent employ 1.5 million staff, care for more than 1 million patients a day and control £150 billion of public expenditure. We promote collaboration and partnership working as the key to improving population health, delivering high-quality care and reducing health inequalities. For more information visit www.nhsconfed.org
About CF
We are a leading consultancy dedicated to making an enduring impact on health and healthcare. We work with leaders and frontline teams to improve health, transform healthcare, embed life science innovation and boost growth through investment. With unmatched access to UK healthcare data and award-winning data science expertise, our team are a driving force for delivering positive and meaningful change. https://www.carnallfarrar.com/
To find out more about this report, or any of our work at CF, contact us today.







