NHS: from competition to collaboration
The 2022 Health and Care Act established Integrated Care Systems, formalising the requirement for an integrated approach to health and care that caters to the population’s needs at scale.
This reflects a growing recognition that collaboration between NHS bodies is important to:
- Progress integration of services across organisational boundaries to provide person-centred holistic pathways of care
- Increase resilience of services and optimal resource allocation across systems, and
- Address unwarranted variation, disparities in care and health inequalities by working at scale
With the establishment of ICSs, health and care organisations are embracing increased collaboration, through both ad hoc responses reacting to emerging opportunities and more structured and strategic initiatives with formal governance structures, to tackle shared challenges and realise opportunities across services and providers.
CF have increasingly been working across the country with systems, collaboratives, and providers to identify opportunities for collaboration, their benefits, and their conditions for success. From our work, which has included substantial stakeholder engagement across multiple different partnerships, we have identified consistent emerging themes in terms of the key challenges and critical success factors to consider when embarking on a collaboration.
Recurring challenges in collaboration
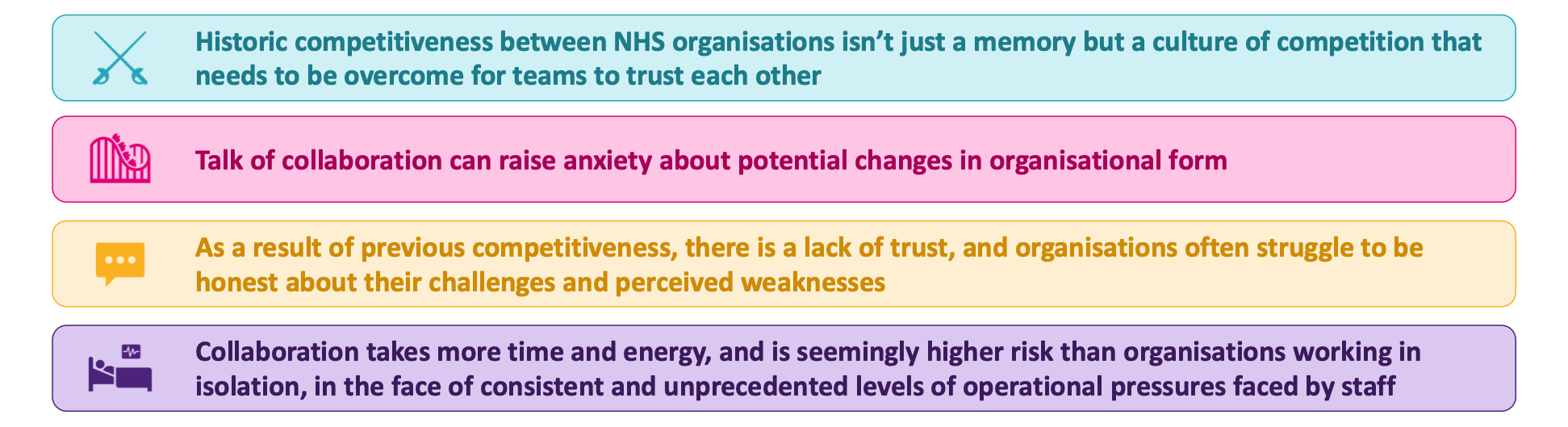
Figure 1: Recurring challenges we have seen when supporting collaboration
Historic competitiveness between NHS organisations remains embedded in staff memory
Whilst collaboration is a key priority for the NHS, a historical emphasis on encouraging competition between providers has left a significant impact. Competition with neighbouring Trusts remains ingrained in the culture of many organisations and in the memories of established staff, with the language of ‘win’ and ‘lose’ permeating the interactions between them. We often see whilst some staff are able to perceive the strategic value of collaboration, others, typically those who have had longer tenures, can be sceptical of changes. They cite past behaviours that undermine the trust needed between organisations to collaborate on transformational agendas, and have confidence that collaboration will result in a better outcome for all.
Those clinical and operational staff who are enthusiastic about collaboration are often hindered by bureaucratic barriers, different organisational cultures, and ways of working, which combine to stifle their energy and enthusiasm to work in partnership. Intertwined with this is ongoing competition for temporary staff and substantive workforce within the market, which continues to undermine trust between organisations.
As a result of previous competitiveness, Trusts often struggle to be honest about their challenges and perceived weaknesses
To identify the full extent of opportunities for collaboration to the benefit of patients, staff, and organisations, all parties need to understand one another’s starting positions, strengths, and limitations. This can be challenging when one organisation is perceived as ‘stronger’ than another, whether that is a view held by organisations themsleves or the public, breeding mistrust in the process. We use an Appreciative Inquiry methodology (see Figure 2) which enables us to leverage the strengths of each organisation, building on how they can maximise their collective strengths to the benefit of the population they serve. This approach has proved valuable in supporting organisations to align on a single version of the truth, be open about their challenges and identify opportunities.
The word collaboration is used in many different ways; in some instances it is a step on a journey to merger and in some instances it isn’t, which can make it really opaque for staff. This is particularly true between organisations where there is a history of proposed and “defeated” organisational changes. Trojan horse is a phrase often used. Staff may become apprehensive around shifts in culture, ways of working, job stability and organisational restructuring, leading sometimes to counterproductive and obstructive behaviour.
Prioritising collaborative initiatives proves to be challenging due to the consistent and unprecedented levels of operational pressures faced by staff
Whilst the pandemic saw extraordinary collaborative efforts across NHS and VCSE organisations, we have since seen these efforts revert, despite staff’s enthusiasm to build on the progress made. The enduring ramifications of the pandemic, including elective backlogs and patients presenting with increased severity and complexity of conditions, combined with continuing operational pressures, including staff strikes, have led to staff burnout and discontent. They express being overwhelmed and time-constrained to drive collaborative initiatives, especially when hindered by inadequate resources, lack of adequate programme management, and bureaucratic hurdles.
In our experience, Trusts need thoughtfully to consider these challenges and how best to address them as they lay out their collaborative agendas. Undertaking meaningful engagement with a wide cross-section of staff is important to uncover the experience of those on the frontline of partnerships and identify what enablers need to be in place to further a collaborative agreement.
Effective collaboration is still possible, but there are a number of critical success factors to be considered
- Quality of care is a unifying force and keeping it as the central tenant and what can be improved for patients, their families and for the population’s health more broadly is key to progressing any discussion and keeping it objective.
- The benefits the collaboration is seeking to realise need to be tangible and resonate for staff – they need to be able to see what could be working better by working differently to justify the effort required to drive initiatives.
- Remove friction for staff as they begin joint working, such as ensuring easy access to buildings, having interoperable data and digital environments, and creating access to patient records across sites and shared training platforms. This makes staff feel valued and working across organisations is seamless, which enables participation, motivation and alignment with the vision for collaboration.
- Governance of collaboration should enable adequate decision-making powers with clear accountability, and a forum empowered with the authority to make timely decisions, mitigate risks, and address conflict. This needs to be jointly owned.
- Effective collaborative ventures require resource. This includes the capacity to manage a programme of work and the budgets and resourcing for initiatives, provide programme management support for initiatives, and employ a communications strategy that informs and engages with stakeholders across both Trusts and further.
- Engagement on and communications around collaboration needs to be longitudinal throughout all levels of the organisation, not just at senior level. Acknowledging challenges within and between the Trusts and assessing on-ground dynamics between partnering colleagues is required to build trust in the process and reduce any fear or anxiety.
- Cultivating organisational development and improving culture across organisations can help to address longstanding behaviours that impede collaboration.
Empowering collaboration has benefits for patients allowing them to receive seamless, patient-centred care at the right place and right time, for staff to gain exposure and training across multiple sites with emerging opportunities in research and development, and for NHS organisations themselves to enhance efficiency and ways of working. However, an honest look at the challenges in collaborating needs to be undertaken and thoughtfully addressed for a partnership to have its desired impact.
Bios:
Sagana Thayaparan is a Consultant at CF. Sagana is passionate about improving health systems for safer and higher-quality patient care and brings her clinical background to deliver a range of projects focused on clinical strategy, care model redesign and collaboration work across a range of settings.
Kaitlin Wolcott is a Manager at CF. She has consulting experience with health systems in both the UK and US, with a focus on strategic initiatives including clinical strategy development, building the case for collaboration, and estates planning.




